The overall aims of diet and lifestyle advice in Diabetes is:
- To improve blood sugar (glycaemic) control
- To decrease in the risk of heart disease
- To help reduce blood pressure
- To lower lipid levels (cholesterol and triglycerides)
- To help delay long term complications
- To tackle obesity through diet education and weight management (5-10% weight loss if overweight) through slow steady weight loss (0.5-1.0 kg/wk)
- To increase exercise
Current Diet Recommendations for Diabetes
Current recommendations suggest that people with diabetes should follow a diet where 50% of energy they consume comes from carbohydrate (starches and sugars) with only 10% of total being simple sugars (sucrose). 35% of total energy should come from fats, particularly from monounsaturated fats and 15% of total energy should come from protein. We shall now look at some specifics of these recommendations:
Salt Intake
It is recommended that salt intake should be limited especially in individuals with Hypertension (raised blood pressure). Salt makes the body retain water and if we eat too much salt, the extra water stored in your body raises your blood pressure. It has been suggested that salt intake should be limited to 6g/day. This can be difficult because 80% of the salt we consume comes from processed foods like bread, biscuits and breakfast cereals, and prepared ready meals or takeaways. Only 20% comes from the salt we add while cooking or at the table. People will therefore need assistance to help them to read labels and identify foods that are high in added salt. As a general rule foods are low in salt if they contain 0.25g salt or less per 100g of food. They contain a medium amount of salt if they have 0.25-1.25g salt per 100g of food and are high in salt if they have 1.25g salt or more per 100g of food.
Fibre
Intakes of fibre rich foods should be increased especially those that are high in soluble fibre such as oats, legumes (peas, kidney beans, and lentils), barley, oats, fruits (such as apples), some green vegetables (such as broccoli) and potatoes. Soluble fibre may help control blood sugar by delaying gastric (stomach) emptying, retarding the entry of glucose into the bloodstream and lessening the rise in blood sugar levels that occurs after eating. The cholesterol-lowering effect of soluble fibres may also help those with diabetes by reducing heart disease risks. According to current guidelines, healthy adults should consume at least 18g of fibre a day.
Exercise
Exercise should be encouraged. Exercise is an important way to manage diabetes as it helps promote beneficial weight loss and also lowers blood sugar levels and helps insulin work more efficiently. Patients treated with insulin will need advice to prevent their blood sugars from dropping too low when they exercise. Emphasis should be placed on the benefits of regular exercise 20-30 minutes 5 times a week.
Carbohydrates
Carbohydrate (from starches and sugars) raises post meal blood sugar levels more than any other nutrient. This observation led to the use of very low carbohydrate diets before insulin and other medication therapies were available. With the advent of these therapies the avoidance of carbohydrates is no longer recommended. Instead, people with diabetes should receive accurate information on which foods contain carbohydrate and how to balance medications with the times when carbohydrates are eaten and the amounts that are eaten.
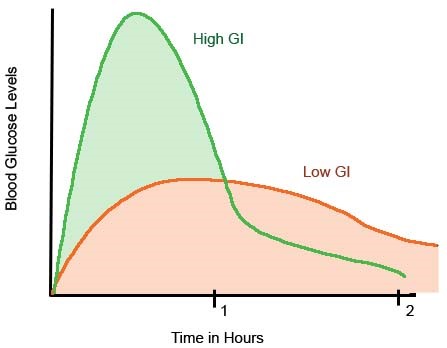
In addition, it is now known that not all foods containing carbohydrates raise blood sugars in the same way. For example 30g of carbohydrate from bread does not have the same effect as 30g of carbohydrate from fruit or as pasta. This is where the Glycaemic index (GI) diet comes into play (Figure 2). The GI is effectively a way of ranking carbohydrate-containing foods according to the extent to which they raise blood sugar levels after eating. Foods are ranked on a scale 0 to 100, 100 being the response to a food of reference like glucose or white bread. Depending on their ranking, foods are labeled as High, Medium or low GI.
It has been proposed that increasing the intake of low G.I. foods will:
- Improve short and long term glucose control
- Improve insulin sensitivity
- Decrease diabetic medication requirements
- Facilitate weight loss
- Increase satiety (the feeling of fullness after meals)
- Reduce risk of heart disease
The general rules for following a low GI diet are:
- To choose whole foods rather than processed
- To eat more whole grain foods
- To eat more fruits and vegetables- aim for 5 servings/day
- To eat more pulses, peas, beans, lentils and sweet corn
- To include a slow release carbohydrate food at each meal
Low GI diet planning-diet advice
Breakfast:
Suggest the use an oat based breakfast cereal and add some fruit. Other low GI cereals include muesli and All Bran
Lunch:
Suggest the addition of baked beans to jacket potatoes. Advise to choose a soup containing lentils and other pulses and try a variety with different breads, e.g. pitta bread and bread made with mixed grains and pumpernickel.
Dinner:
Pasta, noodles and basmati rice are slow release starchy foods. Also advise the inclusion of more beans and pulses. People should be advised that combining foods with different GIs alters the overall GI of a meal, so it is helpful to include a low GI food with each meal.
Snacks:
People should get into the habit of eating fruit as a snack. Other low GI choices include yoghurt, popcorn, rye bread and fruit loaf.
Special Diabetic Foods and Artificial sweeteners
There are many “special” foods marketed specifically to people with diabetes e.g. diabetic cake, diabetic chocolate and diabetic jam. These products contain bulk sweeteners like fructose or sorbitol in place of natural sugar. The value of these products is, however, questionable. A diabetic diet can include some sugary ‘treats’ as part of a balanced diet. Diabetic foods are can also be expensive, may have a laxative effect and can still increase blood sugar. Artificial sweeteners may, on the other hand, be a useful sugar substitute for people with diabetes as well as people who are trying to lose weight.
Examples include: saccharin, neotame, aspartame, sucralose, stevia and acesulfame potassium (Ace-K) These artificial sweeteners are calorie free and can make food taste sweet without raising blood sugar levels.
Course Extract from Nutrition for Disease Management course by Health Academy Australia


excellent and outstanding blog site. I really intend to thanks,
for providing us much better info.