
Unfortunately in our modern time of so many technological breakthroughs it still does not preclude exposure to trauma. Sexual abuse, physical abuse, natural disaster, urban violence, school violence, and terrorism result in significant numbers of people presenting with posttraumatic stress disorder (PTSD) symptoms. In this paper I will be comparing and contrasting PSTD and the Resistance Phase of the GAS and the biochemical and neuroanatomical changes that occur. It also investigates into what possible stress management techniques would be useful in posttraumatic stress disorder and the protocols of treatment that could help to address some of the symptoms of this disorder.
Change is the only thing certain in life. Our lives are constantly moving and evolving. Many times it is in directions that are not by our choice. The change that occurs with a traumatic event can be a slight momentary shift or a gigantic and radical movement from one point to another within us. Sometimes when the changes come in an unsuspected manner or in a violent way it can create stress. If the event is perceived as threatening then it can be categorized as a stressor. This broad term has been used a lot in the past decade and is now showing up in the vocabulary of children. Just the other day my niece who is eight was saying how stressful her life is with all the activities such as ballet, poms, and school. Stress can be a healthy thing or an impacting deleterious event or trauma. It is in this paper that I examine two facets of the outcomes of stress “Post Traumatic Stress Disorder (PTSD) and the Resistance Phase of the General Adaptation Syndrome (GAS). We will compare and contrast the two in their physiology of the body, and also discuss how stress management techniques may benefit clients with PTSD and improve their health outcome.
Post-Traumatic Stress Disorder (PTSD) has had quite a lot of media coverage in the last decade, especially with the events that occurred on September 11 and the other events happening throughout the world. There is a lot of interest into the basic understanding of the impairing effects of PTSD, assessment tools, and treatment options. More and more research and funding are being committed to this topic. PTSD is defined as a potentially debilitating psychiatric condition that can occur after experiencing, witnessing, or being confronted with events involving actual or threatened death or serious injury (Shin et al 2004). But not everyone who experiences or witnesses events that are serious develops the pathology of this disorder. The aetiology of PTSD is multi-faceted.
Persistent symptoms of increased arousal: Difficulty falling or staying asleep; unusually alert and easily startled; difficulty concentrating; increased irritability and anger, that a PTSD patient may experience, can be facilitated by stress management techniques (Brock and Cowan 2004). Sleep complaints and disorders are common in posttraumatic stress disorder (PTSD) (Fagan 2004). In this area there are many preventative measures that can be taken such as establishing a regular sleep routine, using relaxation methods, and maintain realistic self- talk about sleep (Schafer 2000). Just making one’s environment more quiet and peaceful in the evening could be a way for someone to relax and prepare for bed.
The client could also learn to monitor their early warning signs and when they feel like they are being triggered they can use a technique to quite themselves down. Another very simple technique is turning one’s attention to one’s breath. This moves us naturally toward relaxation and meditation, putting one in conscious touch with one’s vital, non-physical essence. Breathing exercises can increase in productivity empowering the person with a strong grounding ability enabling them to control the onset of panic, which is important in the PTSD patient.
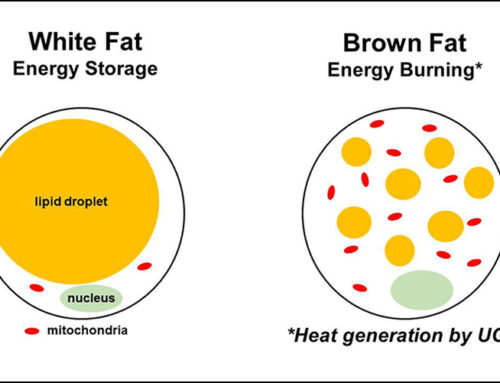
One of the best and most helpful ways would be for the patient to develop and initiate health buffers. Things like getting regular exercise, eating well, resting, and developing healthy pleasures would be assets rather than destructive habits of drowning oneself in alcohol and numbing with drugs. This healthier lifestyle would support the patient in their time with PTSD and beyond.
So-called alternative or complementary therapies are approaching PTSD differently to affect a release of stored emotions and resolution of them, by working with the body, rather than merely talking through the experience. One specific psychotherapeutic approach is Somatic Experiencing (SE), developed by Dr.Peter Levine. SE is a short-term, biological, body-oriented approach to PTSD, or other trauma. This approach heals the person by emphasizing physiological and emotional responses, without re-traumatizing the person, without placing the person on medication, and without the long hours of conventional therapy (Levine 1997). The therapy involves allowing that trapped energy created by the “immobility response” (or paralysis of fight or flight) to be released, while avoiding the cathartic reliving of the immobility which can be re-traumatizing.
Conclusion
In conclusion, the present study shows the effects on the system from the stress related incident. Glucocorticoids play the biggest part by being the effectors to the body accounting for many of the pathophysiology with occurs with PTSD and the Resistance Phase. The studies have shown that the alterations and reactions to the hippocampus and the immune system, which occur via glucocorticoids, have a marked effect on the individuals with PTSD. In relation to treatment and PTSD, many of the symptoms can be lessened with stress management techniques to help the individual come back to a more relaxed and centred internal environment.
By Health Academy Australia
Health Academy offers online fully flexible courses in Aged Care, Nutrition, Psychology, Counselling, Human Biology and Medical Terminology. The courses have full expert tutor support and are accredited. To see all the courses available please visit www.healthcourses.com.au or email admin@healthcourse.com.au


Leave A Comment