Introduction:
Atherosclerosis can be defined as the build up of plaque in the inner part of the arterial walls. Plaque is made of a variety of substances that clog the lining of an artery. This includes deposits of fatty substances, cholesterol, cellular waste products and calcium. As arteries carry oxygenated blood to the heart, the narrowing of these vessels can lead to a decrease in blood to the heart, which can cause numerous problems and can be fatal.
Eventually plaques will grow large enough to be able to obstruct the flow of blood through a vessel; however the damage is caused when the plague breaks away forming clots or Thrombi in various different positions in a vessel. A thrombosis is simply the formation of a clot inside a blood vessel that obstructs its flow. Problems for these clots depend on their location. If they are present in the coronary artery of the heart, this decrease in blood flow could lead to a heart attack which is medically termed a Myocardial Infarction or MI. A myocardial infarction occurs when there is a prolonged decrease of oxygen (Ischemia) that will eventually lead to tissue death. Infarction refers to necrosis or death of myocardial cells. Atherosclerotic heart disease is the most common cause of MI.
Peripheral emboli are the name given to describe objects that migrate from one part of the body and cause a blockage or occlusion elsewhere. If the obstruction occurs in an artery that supplies oxygen and blood to the brain, it could cause a stroke. Gangrene is often a complication that is common when there is blocked blood flow to the body’s extremities, the hand and legs.
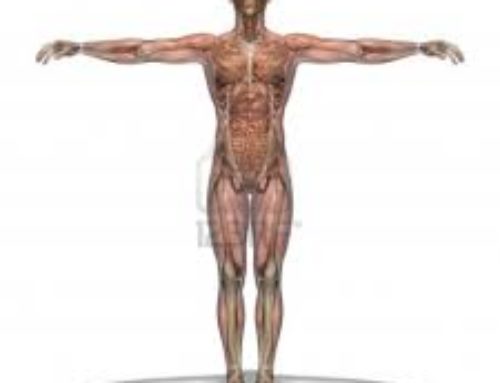
Atherosclerosis can affect any artery anywhere in the body therefore a number of different complications could arise, depending on the position of the artery affected.
Atherosclerosis of the coronary arteries in the heart is the leading cause of death in the United States. Atherosclerotic blocks to other parts of the body causing stroke and other diseases is the third most common cause of death after cancer.
Causes:
Some people are more at risk than others in developing atherosclerosis. The repeated insult to the walls of the arteries is the primary cause of developing this disease. Some of the known risk factors include:
- High blood pressure or hypertension
- Diabetes Mellitus
- Insulin Resistant
- Smoking
- Alcohol Intake (less than 14 drinks per week for men & less than 9 drinks per week for women)
- Chemical Abnormalities/High cholesterol levels in the blood
- Obesity
- A sedentary life style
- A family history of heart disease
- Stress
- Depression
- Male Gender
- Older aged people
- Lowered Oestrogen levels post menopause
- Infections: bacterial or viral eg: Chlamydia Pneumoniae or cytomegalovirus
Damaged artery walls release chemicals called monocytes and T-cells which attach to the lining of the vessel, this generally occurs where the artery branches. These cells then change and are called Foam cells. These are the cells that are responsible for attracting the cholesterol and other fatty substances in the blood which later accumulate calcium and become plaques. The plaques cause the narrowing of the blood vessel and therefore decrease the flow of blood through the vessel. The rupturing of these plaques will release material that triggers clot formation elsewhere in the vessel and is the leading cause of heart attacks and stroke. The plaque itself can also be responsible for the occlusion of vessels when its pieces are fragmented to various locations of the vessel.
Signs and Symptoms:
Atherosclerosis unfortunately, has no progressive symptoms until the damage to the arteries has already occurred. The symptoms are recorded to present when the artery is 70% occluded
Once the vessels have been damaged the following symptoms may be present:
Claudication: Pain in the calf brought on by walking and generally relieved by resting.
Angina: Chest pain, due to the restricted blood flow to the heart muscle
Myocardial Infarction: Heart attack.
A decrease in supply of blood to vessels of the brain may cause a stroke and therefore signs and symptoms of a stroke will be seen. Symptoms of dizziness and nausea may be noticed and last for less than 24 hours.
Diagnosis:
Atherosclerosis is normally diagnosed after other symptoms have presented themselves and Coronary Artery Disease (CAD) is suspected and diagnosed. A non-invasive examination by a physician could detect a ‘bruit’, (a whooshing/blowing sound) over the artery with the use of a stethoscope. The risk of heart disease can be detected by examining a blood sample. Elevated levels of cholesterol, triglycerides and the blood clotting factor are areas of concern when a blood sample is analysed.
Other diagnostic tests include:
Angiogram or Arteriogram: This is a medical image, using x-rays pictures that are taken to visualize arteries, veins and heart chambers/coronary arteries. A catheter is used to administer a radiocontrast agent into the artery, generally in the groin or forearm area and is then advanced all the way to the coronary arteries. A presence of atherosclerosis /atheroma in the walls of an artery is clearly identified. It is the most accurate method of detecting the severity of the condition.
CT Scan (Computerised Tomography): This procedure usually takes an hour and is compiled by a computer that picks up x-rays that are sent through the body at various different angels to get a cross section of the area under investigation. A very fast CT scan using and Electron Beam (EBCT) is then used to directly visualize the arteries and measure the amount of calcium in the vessel. This provides the necessary evidence that suggests there is plaque in the artery and is a non-invasive method of testing.
Electrocardiogram (ECG) / Stress Test: This non-invasive technique is used to view the hearts electrical waves and is normally suggested with patients that suffer chest pain during exercise. Any heart abnormalities are monitored at rest, then during stress (walking on a treadmill) and again during recovery. If the patient is unable to physically walk or run, then drugs such as dobutamine and adenosine can be administered to mimic the stress of the heart. Blood pressure is also monitored closely before, during and after the test. Other stress tests involve echocardiography and radioactivenucleotide markers that can image the heart and the sounds of the heart to detect any stress related abnormalities. These tests can only suggest if there are any blockages however a coronary angiogram is the gold standard in confirming the block and its placement.
Complications:
The most common complications of atherosclerosis are:
- Decrease bloody supply to regions resulting in ischemia and angina.
- Aneurism
- Stroke
- Kidney failure
- Abnormal Heart Rhythms
- Damage to organs, muscles and vessels.
- Decrease sensitivity in the body’s extremities due to poor circulation.
- Gangrene (rare)
- Death
Treatment:
Treatment will generally commence once a complication such as heart attack or chest pain has occurred. Treatment can be both surgical and non-surgical.
Non-Surgical Treatments:
Angioplasty: This surgical procedure improves blood flow by the insertion of deflated balloon using a catheter. This balloon is then inflated allowing the blood to flow freely through the vessel. In some cases a permanent placement of a wire mesh called a stent is inserted to widen the artery to increase the blood flow. Stent placement surgery is considered the most affected way to deal with atherosclerotic vessels
Laser Revascularization: Use to relieve chest pain if no other treatments have succeeded. This treatment involves creating multiple channels in the heart allowing a better flow of oxygen and nutrients to the muscle.
Atherectomy: Removal of plaque from the inner walls of the artery.
Surgical Treatments:
Bypass Surgery: Surgery involving the redirection of blood from clogged arteries to increase the flow of blood. This procedure can also be done with smaller incisions in the chest as opposed to regular bypass surgery.
Endarterectomy: Procedure involving the removal of plaques from the carotid artery (the artery in the neck where you normally record your pulse)
Drug Treatments:
- Blood pressure lowering drugs such as: Beta-Blockers, Angiotensin and Calcium Channel Blockers.
- Cholesterol Lowering drugs such as: Niacin’s and Statins.
- Blood thinning Drugs: Aspirin often given to people with an MI
- Nitrates
Gene therapy has been identified in being a potential treatment for atherosclerosis.
Alternative Treatments:
- Homeopathy
- Massage
- Exercise
- Acupuncture
Prevention:
Like most diseases, the best prevention is being vigilant with your life choices. A diet low in cholesterol, saturated fat and sodium will prevent the body developing plaques and reduce the chances of developing high blood pressure. Physical activity improves circulation and allows your muscles to use oxygen more effectively. Smoking is one of the quickest ways to damage the walls of your vessels. Quitting smoking will significantly reduce the progression of further damage to the vessels and is a serious component in the prevention of this condition. Stress will contribute to all the symptoms of this disease and can be maintained using different techniques such as breathing and yoga which will aid in maintaining a healthy mental and physical equilibrium.






Leave A Comment