
Introduction
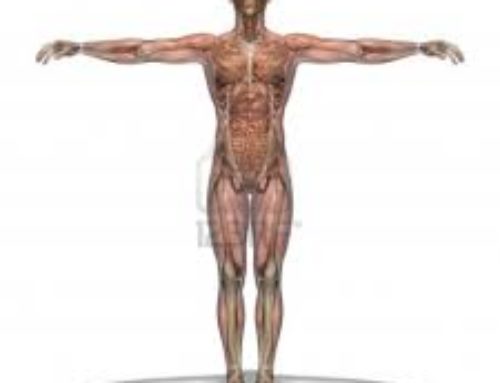
Bursitis is the inflammation of a bursa, the small fluid filled sac which cushions the point of contact near joints. There are 160 bursae in the body. The major bursae are found next to the tendons near the large joints, such as the shoulders, elbows, hips, and knees. Bursitis is most commonly caused by overuse of a joint, or from repeated pressure or tension on the joint for extended periods of time.
As you get older, you are more likely to develop bursitis in one of your joints.The most common joint for bursitis is the shoulder, as it has the greatest range of motion of all the body’s major joints. Other people who are at risk for bursitis are typically involved in intense athletic activity. In addition to athletes, people who suddenly increase their activity level when out of shape can cause an acute bursitis to develop. Care must be taken not to over-exert, or to increase the intensity of your training too quickly.In addition, certain diseases and conditions increase your risk of developing bursitis, such as:
- Arthritis
- Gout
- Staphylococcal infection
- Tuberculosis
Sign and Symptoms
To diagnosis bursitis, the doctor will perform a comprehensive physical examination, looking for tenderness in the area of the pain. The most common signs and symptoms of bursitis are inflammation, swelling and pain in the area particularly during stretching or extension when exercising, lifting or otherwise pushing the joint beyond its normal limits. Some people report restricted range of motion in a joint, with or without immediate pain. It is also common for the overlying skin may become red or feel warm.The doctor may also perform additional tests to rule out other possible injuries or conditions. These tests may include radiography (x-rays), bone scanning, and magnetic resonance imaging (MRI). X-ray testing can sometime detect calcifications in the bursa when bursitis has become chronic or recurring.
Causes
Bursitis can occur at any age but usually occurs in older individuals and is related to an inflammatory joint disease such as rheumatoid arthritis or gout, or recurring trauma that stresses or pressures a joint. People in poor physical condition and those who have bad postures are also at risk of developing this condition. Injury or overuse is what usually causes bursitis. Another way that bursitis occurs is when compression of the bursa happens on a regular basis, such as a side sleeper who places significant pressure on the shoulder or hip when they lay down for long periods. In this case it would not take too much movement of this already compressed area to cause friction of the bursa. It may also occur by using an affected limb incorrectly. Chronic bursitis follows attacks of acute bursitis or repeated trauma and infection. Septic bursitis may result from wound infection or from bacterial invasion of skin over the bursa. Occasionally the cause of bursitis can not be determined.
The type of bursitis that affects each person varies. Some of the more common types are outlined:
Anterior Achilles tendon bursitis
This type of bursitis is caused by extra strain on the Achilles tendon and is often referred to as Albert’s disease. It is characterized by inflammation of the bursa located in front of the attachment of the tendon to the heel and often caused by wearing shoes with a rigid back.
Posterior Achilles tendon bursitis
Otherwise called Haglund’s deformity, it refers to the inflammation of bursa located between the skin of the heel and the Achilles tendon, which attaches the calf muscles to the heel. Walking which places pressure on the soft heel tissue against the hard back support of the shoe, aggravates and leads to this type of bursitis. It most often occurs in young women as a result of improper footwear, prolonged walking or in sports, such as ice-skating.
Hip bursitis
The anatomical name is trochanteric bursitis. It is often the result of injury, overuse, spinal abnormalities, arthritis, or surgery. The pressure from standing or sitting for a prolonged time also may lead to bursitis of the hip. This type of bursitis is also more common among women middle-aged and older people.
The following risk factors have been associated with the development of hip bursitis.
- Bone spurs or calcium deposits. Often develop within the tendons that attach to the trochanter, the spurs irritate the bursa and cause inflammation.
- Repetitive stress (overuse) injury. This can occur when running, stair climbing, bicycling, or standing for long periods of time.
- Leg length inequality. When one leg is shorter than the other by more than an inch or so, it affects the way you walk and can lead to irritation of a hip bursa.
- Spine disease. Including arthritis of lower (lumbar) spine, scoliosis and other spine problems.
- Rheumatoid arthritis. This condition makes the bursae more prone to becoming inflamed.
- Previous surgery. Surgical scars around the hip or prosthetic implants in the hip can irritate bursae and cause bursitis.
Elbow bursitis
This type of bursitis is caused by the inflammation of the olecranon bursa located between the skin and bones of the elbow. It often results from injury or constant pressure on the elbow doing something as simple as like leaning on a hard surface. This type of bursitis is associated with actions requiring you to repeatedly bend and extend your elbow such as by pushing a vacuum cleaner back and forth. Other examples of repeated physical activities that may lead to bursitis or tendinitis of the elbow or shoulder that include throwing a baseball and swinging a tennis racket or a golf club.
Knee bursitis
Commonly known as Pes Anserine bursitis or goosefoot bursitis, the affected bursa in this case is located between the shin bone and the three tendons of the hamstring muscles, on the inside of the knee. This is usually caused by lack of stretching before exercise, tight hamstring muscles, arthritis, being overweight, or outward-turning of the knee or lower leg.
Kneecap bursitis
Medically known as prepatellar bursitis, this form of bursitis, involves the soft, egg-shaped bump occurs on the front of your knee, and is common among skilled labourers like carpet layers and plumbers, who need to sit on their knees a lot. A sharp blow to the knee can cause inflammation of the bursae around the kneecap. People with arthritis who are overweight often develop bursitis of the knee.
Shoulder bursitis
Bursitis of the shoulder often results from injury to the rotator cuff, the muscles and tendons that connect your upper arm bone to your shoulder blade. Causes of the bursitis may include falling, lifting and repetitive overhead arm activities. Sometimes it’s hard to distinguish between the pain caused by bursitis and that caused by a rotator cuff injury.
Complications
Severe or long-lasting bursitis can lead to reduced movement or use of the joint and result in muscle atrophy (wasting). Permanent changes in the shape of the bursa, such as thickening or enlarging can occur and the surrounding tissues can become chronically inflamed. If the bursitis is associated with tendonitis, then tendon rupture is a possible complication. However the main complication of bursitis is an infection of the bursa.
Possible treatment methods
Treatment of bursitis depends on whether or not infection is involved.
If no infection is suspected then treatment aims to alleviate the symptoms as much as possible while the healing process takes place. If the bursitis was triggered by overuse, avoiding the particular activity is crucial.Treatment options initially focus on Rest, Ice, Compression and Elevation (RICE). The ice will help to control the inflammation and decrease swelling. By minimizing inflammation and swelling, the bursa can return to its usual state and perform its usual function. Trying to rest the joint by immobilization with a sling, splint or cast will help keep pressure off of the affected area and allow time to heal.
Nonsteroidal anti-inflammatory medications (NSAIDs) include a long list of possibilities such as Ibuprofen, Motrin, Naprosyn, Relafen, Lodine, Daypro, Mobic, Celebrex, and many others. Bursitis treatment can be improved by these medications that will decrease pain and swelling. Be sure to talk to your doctor before starting these medications. If the symptoms of bursitis are persistent, an injection of cortisone may be considered. Cortisone is a powerful anti-inflammatory medication, administered via injection directly to the site of inflammation. This can be extremely helpful for situations that are not improved with rest.
Infectious or septic bursitis requires even further evaluation and aggressive treatment. Septic bursitis is caused by the presence of a pus-forming organism, most commonly staphylococcus aureus. Diagnosis of infection is confirmed by examining a sample of the fluid in the bursa and requires treatment with antibiotics taken orally (by mouth), injected into a muscle or into a vein (intravenously). The bursa will also need to be drained by needle two or three times over the first week of treatment. When a patient has such a serious infection, there may be underlying causes such as an inefficient immune system or undiscovered diabetes.
Self-care for bursitis
Proper strengthening technique can help you avoid bursitis by using your muscles in a safe, more efficient manner. For example, patients with shoulder bursitis can learn ways to move the shoulder that will not cause inflammation. An adequate warm-up before and correct posture during exercise is useful.
Medical treatment of bursitis
Splinting and casting may rest the joint by limiting its motion, but should only be done under the supervision of a doctor or physiotherapist.
Anti-inflammatory and analgesic medications may be prescribed to reduce pain and inflammation.
Diathermy, or deep-heat therapy, which can relieve the discomfort and inflammation of bursitis, is gaining popularity. It can also soothe tense muscles, nerves and tendons.
In severe or recurrent cases, bursal drainage may be performed. This procedure involves the removal of the fluid with a needle and syringe under sterile conditions. This procedure is referred to as aspiration of fluid. It can usually be performed in the doctor’s rooms. Repeated aspiration of the inflamed fluid may be required. Long-term control of chronic bursitis may require changes in lifestyle to prevent recurring joint irritation.
Surgery is sometimes necessary to remove a thickened bursa that has not improved with any other treatment. Surgical removal is usually done because the swollen bursa is restricting your activity. Bursectomy involves the surgical removal of the affected bursa is removed, though this is very rarely undertaken. Generally, the adjacent joint functions normally after the surgical wound heals.
Alternative therapies
Alternative treatments take into consideration the role of diet in causing bursitis. Contributing issues include the misuse of calcium by the body, magnesium deficiency, and food allergies. Vitamin supplements and diet changes may be helpful. The use of homeopathy, aromatherapy, herbs and hydrotherapy may help relieve symptoms, such as ginger is reportedly useful in reducing inflammation. While it has been proven that acupuncture is effective in treating hip and shoulder pain caused by bursitis and other conditions. Other therapies that can effectively deal with musculoskeletal problems may also be helpful, such as magnetic field therapy, naturopathic medicine, applied kinesiology and chiropractic.





Leave A Comment