
Introduction
Mitral valve prolapse is a displacement of the mitral valve when the heart contracts. This is also commonly called “floppy” mitral valve or “Barlow’s syndrome. It is the most common heart valve abnormality, affecting five to ten percent of the world population.
Mitral valve prolapse has a strong hereditary tendency, although the exact cause is unknown. Affected family members are often tall, thin, with long arms and fingers, and straight backs. It is seen most commonly in women from 20 to 40 years old, but also occurs in men.
Unfortunately, it is also one of the most commonly misunderstood – both by patients and their doctors.
Causes
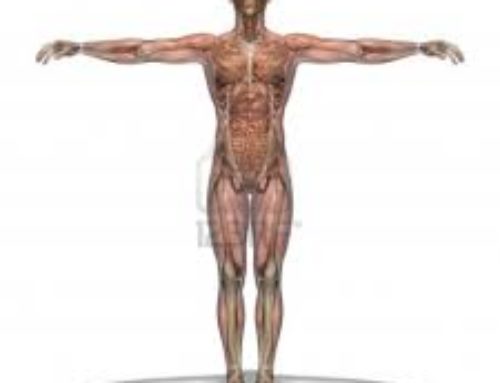
Understanding the heart circulation helps to understand how mitral valve prolapse occurs. The heart is divided into 4 chambers. These chambers fill with blood, which is then pumped throughout the body to supply nourishment. To assist this pumping action the four valves open and close. This allows the blood to move in a forward direction. The mitral valve is a heart valve made of 2 tissue flaps, called leaflets, which open and close. The mitral valve is located between the left atrium and the left ventricle of the heart. Mitral valve leaflets are shaped like parachutes and attach to the inner wall of the left ventricle by a series of strings called “chordae.” When the ventricles contract, the mitral valve leaflets close snugly and prevent the backflow of blood from the left ventricle into the left atrium. When the ventricles relax, the valves open to allow oxygenated blood from the lungs to fill the left ventricle.
A deformity in the mitral valve can keep the leaflets from closing well. Most patients are totally unaware of the prolapsing of the mitral valve. Sometimes small amounts of blood may flow backward in your heart, this is referred to as mitral regurgitation. Severe mitral regurgitation can lead to heart failure and abnormal heart rhythms.
Sign and Symptoms
In its mild form most patients with mitral valve prolapse are asymptomatic.
While in the more serious form patients with mitral valve prolapse may report any of the following symptoms:
- irregular heartbeat or palpitations
- Shortness of breath
- tachycardia, or increased heartbeats and pounding in the chest, often occurring after exercise
- chest pain that can last from seconds to hours, often when you are resting
- panic attacks such as a sudden feeling of anxiety or doom
- fatigue, dizziness, and weakness, sometimes misdiagnosed as chronic fatigue syndrome
- blood pressure that falls below normal when you stand up, causing lightheadedness
- mitral regurgitation and
- infective endocarditis.
Patients can also present with numerous nervous system symptoms including panic attacks, anxiety, fatigue, migraine headaches or depression. Further co-occurring illnesses such as Marfan syndrome or hyperthyroidism is common.
Always seek medical advice if symptoms persist or are recurrent, such as chest pains that come and go, palpitations, or light-headedness.
Complications
Complications of mitral valve prolapse are rare. The most commonly reportedly complications for mitral valve prolapse includes arrhythmia, mitral regurgitation, bacterial endocarditis and heart failure.
Where mitral regurgitation has been diagnosed, there is an increased risk of acquiring bacterial endocarditis. This complication occurs as a result of bacteria growth which is attracted around the deformed mitral valve flap.
Diagnosis
The diagnosis of mitral valve prolapse in asymptomatic patients is often made by auscultation of the heart, which is listening to the heart beat and performed using a stethoscope. The most frequent presenting complaint is palpitations, the usual source being premature ventricular beats. Using a stethoscope, a clicking sound is heard soon after the ventricle begins to contract. This clicking is felt to reflect tightening of the abnormal valve leaflets against the pressure load of the left ventricle. If there is associated leakage (regurgitation) of blood through the abnormal valve opening, a “whooshing” sound (murmur) can be heard immediately following the clicking sound.
The most useful test for mitral valve prolapse is an echocardiogram. This test uses sound waves to create a moving picture of your heart. It provides information about the shape and size of your heart. In addition the test also can identify areas of poor blood flow to the heart, areas of heart muscle that are not contracting normally, and previous injury to the heart muscle caused by poor blood flow. The echocardiogram is a painless test that’s used to look for prolapse of the mitral valve flaps and for regurgitation or backflow regurgitation of blood through the leaky valve. The information gathered by an echocardiography can measure the severity of prolapse and the degree of mitral regurgitation.
Treatment
Specific treatment for mitral valve prolapse will be determined by your physician based on your overall health and medical history, the extent of the disease, your signs and symptoms and your tolerance for specific medications and procedures.
Treatment approaches fall under two main categories depending on when the patient presents with no symptoms or asymptomatic, or presents with symptoms or symptomatic.
Asymptomatic Patients
Most people with mitral valve prolapse are asymptomatic and not at high risk for serious consequences therefore rreassurance is the major component in the management. Patients with few or no symptoms and mild mitral valve prolapse should be reassured of their benign prognosis. Regular exercise and a healthy lifestyle are highly encouraged. The vast majority of patients with aymptomcatic mitral valve prolapse can expect to lead completely normal lives, without any symptoms due to their mitral valve prolapse and without any decrease in longevity.
Symptomatic Patients
Patients with mitral valve prolapse who present with symptoms predominantly palpitations associated with mild tachyarrhythmias, chest pain, anxiety or fatigue often respond to therapy with beta blockers. The heart rhythm abnormalities in mitral valve prolapse sometimes become very uncomfortable. Beta-adrenergicblockers along with calcium channel blockers and anxiolyticsare widely used to treat symptoms associated with mitral valve prolapse despitea lack of evidence that supports their efficacy (1).
Prolapsed heart valves can become infected more easily than normal valves. Infection speeds up the valve damage and may worsen symptoms. Your provider may prescribe antibiotics to reduce this risk.
Orthostatic symptoms related to postural hypotension and tachycardia are best treated with volume expansion, preferably by increasing salt and fluid intake. Mineralocorticoid therapy may be needed in severe cases. In addition wearing support stockings may also be beneficial.
Very rarely but on some occasions when the valve leakage is severe or prolapse is extreme, surgery may required to repair the valve. Over the last decade improvements in heart surgery have shown less need for mitral valve replacement with an artificial valve.
Once mitral valve prolapse has been diagnosed, call your medical provider if symptoms worsen or do not go away.
Alternative therapies
There are many facets of alternative medicine which can help alleviate
the multiple symptoms experienced by people with mitral valve prolapse. These areas include diet modifications, cognitive therapy and nutritional supplements.
the multiple symptoms experienced by people with mitral valve prolapse. These areas include diet modifications, cognitive therapy and nutritional supplements.
Cognitive therapy is the main ground for the holistic approach to mitral valve prolapse. Therapy requires the patient to comprehend precisely what is happening to their body and learn ways to block the feedback loops that can lead to panic attacks or hyperventilation, and break the cycle. By performing a “reality check,” you can learn to break the conditioned response you have acquired to your own physical symptoms.
Exercise is fantastic for reconditioning and relieving neurological symptoms. Studies have shown that people who engage in regular aerobic exercise report a decline in symptoms of chest pain, fatigue, dizziness and mood swings, and panic attacks.
Proper diet is crucial in controlling the symptoms of mitral valve prolapse. Firstly avoidance of stimulants, sugar, and artificial flavouring agents are mandatory. Whilst intake of moderate levels of salt is usually encouraged to stimulate adrenal function.
The following are key nutrients that can affect the underlying causes of mitral valve prolapse symptoms:
- Magnesium is probably the most significant of these. There is a vast amount of medical research studies from various parts of the world that link mitral valve prolapseto magnesium deficiencies, and/or that show improvement of mitral valve prolapse symptoms following magnesium treatment.
- L-carnitine
- Acetyl-l-carnitine
- Co-enzyme Q10
- Vitamin B6
- Inositol
Natural Relaxants including Kava, Valerian and Hops calms the central nervous system, relaxes muscle tissue and are effective for insomnia.
References
(1). Scordo, K., (2007) Medication use and symptoms in individuals with mitral valve prolapse syndrome. Clinical Nursing Research, Vol. 16, No. 1, 58-71.





Leave A Comment